FHIR Implementation Guide for Stroke - Local Development build (v0.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
Stroke-CP
The BPMN Representation of the Stroke Clinical Pathway (Stroke-CP)
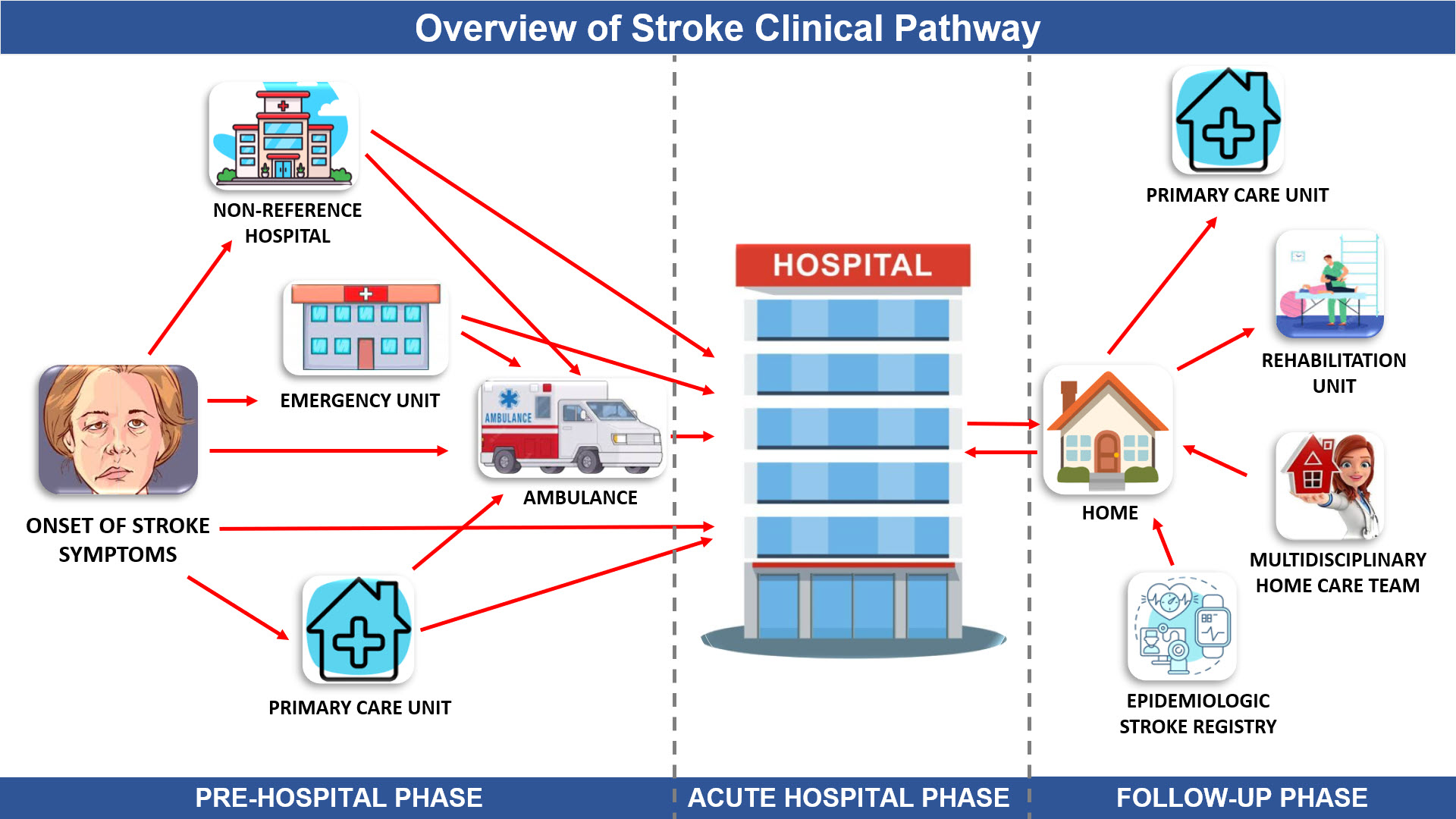
In order to provide a more comprehensive representation of the Stroke Clinical Pathway (Stroke-CP), it has been categorically partitioned into three distinct phases: (1) Pre-Hospital Phase, (2) Stroke Acute Hospital Phase, and (3) Follow-up and Rehabilitation Phase, as visually depicted in Figure 1. The Pre-Hospital Phase encompasses the temporal interval initiating from the manifestation of the onset of stroke symptoms and extending until the point of referral or transfer to the designated referral hospital. The Acute Hospital Phase corresponds to the duration of hospitalization at the referral facility, during which the patient undergoes comprehensive acute care encompassing diagnostic evaluations, therapeutic interventions, specialized monitoring, and continues until the patient's eventual discharge from the hospital. Lastly, the Follow-up and Rehabilitation Phase represents the subsequent period after hospital discharge, wherein the patient's progress is continually monitored, while concurrently receiving post-discharge care, rehabilitation services, and enduring support to facilitate their recovery process.
|
|---|
Figure 1 – Representation and relationship of the phases (a) Pre-Hospital Phase, (b) Stroke Acute Hospital Phase, and (c) Follow-up and Rehabilitation Phase in the clinical pathway for stroke patients.
Pre-Hospital Phase
The Pre-Hospital Phase (Figure 2) consists of six defined pools:
1. Location where the stroke onset symptoms occurred
2. Primary Care Unit
3. 24-hour Emergency Unit
4. Non-Reference Hospital
5. Ambulance
6. Stroke Reference Hospital
Figure 2 – Representation in BPMN of the Pre-Hospital Phase of stroke patient care.
Upon symptom onset at the designated location, patients are faced with the decision: "What Health Unit does the user go to?" This decision delineates five potential trajectories within the Joinville Public Health System: Primary Care Unit, 24-hour Emergency Unit, Non-Reference Hospital, Public Ambulance, and Stroke Reference Hospital. Each trajectory is mirrored by a unique pool. The pools for the Primary Care Unit, 24-hour Emergency Unit, Non-Reference Hospital, and Stroke Reference Hospital are partitioned into three lanes. These lanes depict the sequential engagements of the Receptionist, Nurse, and Physician. During each interaction, specific data points, highlighted in green and inclusive of both process data and ICHOM data, should be integrated into the Electronic Health Record. Although the 24-hour Emergency Unit, Non-Reference Hospital, and Stroke Reference Hospital exhibit similar processes, there's a key distinction. Those at the Stroke Reference Hospital are ushered to the Acute Stroke Unit, while the rest are directed to the Stroke Reference Hospital. The Primary Care Unit, in contrast, adheres to its unique triage protocol, diverging from the Manchester Protocol prevalent elsewhere. The Ambulance pool stands apart with its two lanes, representing the receptionist and the healthcare professional in charge of emergency care, which may be a doctor, a nurse, or both. Importantly, a pathway highlighted in red delineates the recommended protocol for stroke patient care.
Stroke Acute Hospital Phase
In the reference hospital dedicated to stroke care, depicted in Figure 3, the initial point of contact is the Acute Stroke Unit. This unit, helmed by a multidisciplinary team of physicians and nurses, prioritizes immediate intervention. A salient aspect of this model focuses on the critical role played by the neurologist, especially in data collection following the ICHOM guidelines. Notably, while non-interoperable systems may sometimes present barriers to comprehensive data acquisition at this juncture, the emphasis remains on collecting this data, representing an ideal scenario.
Figure 3 – Representation in BPMN of the Acute Hospital Phase of stroke patient care.
Following a thorough evaluation of the patient's clinical history, the neurologist discerns the need for advanced imaging tests. Primarily, these include the Computed Tomography (CT scan) and the Magnetic Resonance Angiography (MRA), instrumental in classifying the type of stroke and subsequently delineating the optimal treatment strategy. This study predominantly focuses on ischemic stroke treatments, taking into account a therapeutic window of 4 hours and 30 minutes for thrombolysis, and an extended 12 hours for thrombectomy initiation. A pressing question at this stage remains: 'Is there an indication for thrombolytic therapy, thrombectomy, or hemicraniectomy?'
In situations where clinical indicators for the above treatments are absent, the evaluation by the neurologist continues unabated. If a patient's condition is assessed as stable, bed allocation within the Integral Stroke Unit (ISU) becomes a priority. Nonetheless, constraints in bed availability necessitate seeking alternative accommodations within the hospital. Procedures such as thrombolytic therapy are typically administered within the Acute Stroke Unit. In contrast, more involved procedures like thrombectomy and hemicraniectomy warrant the transfer of the patient to specialized surgical facilities. For patients in critical condition, immediate referral to the Intensive Care Unit (ICU) becomes paramount. It's also important to underscore that diagnostic tests, like the CT scan and MRA, are conducted within the dedicated Diagnostic Imaging Department. The average duration within the Acute Stroke Unit hovers around three days.
Post-procedures, especially after Thrombolytic therapy and thrombectomy, patients are closely monitored for potential symptoms of intracranial hemorrhage. If such symptoms manifest, considerations for hemicraniectomy come to the fore. The subsequent phase involves vigilant monitoring of the patient's clinical status. Those deemed unstable are directed to the ICU, where outcomes can range from unfortunate demises to stabilization or significant clinical improvement. Stable patients are subsequently evaluated for bed availability in the ISU. If beds are available, a transfer to the CSU occurs; if not, alternative hospital units come into play.
Within the ISU, patients are ensconced in an environment that promotes holistic care. This care is rendered by a team that spans multiple disciplines – physiotherapists, speech therapists, nutritionists, nurses, and neurologists, among others. During their stay, stringent data collection protocols, consistent with ICHOM guidelines, are implemented. Prior to discharge, the patient's status undergoes another round of evaluation to determine the need for extended care, be it through the Multidisciplinary Home Care Team or through a referral to a long-term care facility for stroke patients. Ultimately, two primary outcomes materialize: either the patient is prepped for discharge to their home or a designated care facility, or they are referred to a Long-Term Stroke Care Hospital. In the realm of stroke care, the treatment standards upheld within the ISU should ideally be mirrored across all hospital inpatient units. However, in many instances, this parity is not observed, leading to potential discrepancies and gaps in patient care. It is noteworthy that the average length of stay within the ISU typically ranges from 5 to 12 days.
Follow-up and Rehabilitation Phase
The Follow-up and Rehabilitation Phase is composed of 7 pools (Figure 4):
1. Stroke Long-Term Hospital
2. Home
3. Primary Care Unit
4. Rehabilitation Unit
5. Reference Stroke Hospital
6. Multidisciplinary Home Care Team
7. Epidemiologic Stroke Registry
Figure 4 – Representation in BPMN of the Follow-up and Rehabilitation Phase of stroke patient care.
The initial pool, labeled 'Stroke Long-Term Hospital,' focuses on the routine monitoring of the patient by healthcare professionals within the Long-Term Care Hospital until one of the outcomes is reached, either hospital discharge or demise. The 'Home' pool encompasses the patient journey from hospital discharge through appointments and follow-ups at the Primary Health Care Unit, Rehabilitation Unit, the Reference Hospital for Stroke, home visits by the Multidisciplinary Home Care Team, and oversight by the Epidemiologic Stroke Registry. Once an intervention at one of these service units concludes, the patient reenters this flow to schedule their subsequent visit.
The procedures within the pools: 'Primary Care Unit', 'Rehabilitation Unit', 'Reference Stroke Hospital', and 'Multidisciplinary Home Care Team' share a consistent operational structure. Initially, the patient is received by the receptionist and subsequently directed to the scheduled healthcare professional, which might include nurses, physicians, physiotherapists, speech therapists, nutritionists, psychologists, among others. Following this consultation, the patient may be directed either to schedule another appointment or to conclude their current care cycle. This sequence recurs in a loop until the patient's treatment concludes.
The 'Epidemiologic Stroke Registry' pool operates on a distinct flow since its primary function is to collate data from stroke patients. This service amasses patient health data using various methods such as phone calls, mobile applications, or other communication mediums. Data collection intervals are set at 30 days, 90 days, and then annually for the first five years post-stroke (ICTUS) event, after which the patient is formally discharged from this monitoring service.